Abstract
The Impact of Glycemic Control in Thrombo-inflammatory Biomarkers in Diabetic Pulmonary Embolism Patients.
Bulent Kantarcioglu, Alexander O'Hara, Jacob Pozin, Roumika Patil, Maddie Allen, Emily Krupa, Fakiha Siddiqui, Debra Hoppensteadt, Atul Laddu, Amir Darki, Jawed Fareed.
Introduction: Venous thromboembolism (VTE) is estimated to affect between 350,000-600,000 individuals annually in the United States. The mortality rate is approximately 100,000 people each year. Diabetes mellitus (DM) is one of the most common metabolic disorders resulting from dysregulated glucose metabolism and is a very important risk factor for cardiovascular disease. Several different factors contribute to thrombotic events in DM; these include inflammatory states, primary hemostatic changes, increased levels of various clotting factors, impaired fibrinolysis, increased oxidative stress, and endothelial dysfunction. However, the results of previous studies were inconsistent to explain the complex relationship between the poor glycemic control in DM and development of PE. HbA1c, which is used as an indicator for glycemic control, may also be an important measurement to quantify the level of thromboinflammatory response that is observed in diabetic patients. Thrombo-inflammatory biomarkers such as D-Dimer, CRP, PAI-1, tPA, TAFI, vWF and endogenous glycosaminoglycans (GAGs) were investigated in several previous studies, however, the relevance of these biomarkers in complex relationships of DM and PE is not completely understood. This study aimed to investigate the role of DM in modulating thromboinflammatory biomarkers in PE patient.
Materials & Methods: The diabetic PE patient samples were collected following the ongoing IRB and PERT protocols at Loyola University Medical Center and affiliated hospitals. The levels of thrombo-inflammatory markers (D-Dimer, CRP, PAI-1, tPA, TAFI and vWF) were tested by ELISA methods, endogenous GAGs with heparin red (Red Probes, Muenster, Germany) method. The clinical information of 113 diabetic PE patients, including the HbA1c levels within 3 months of PE diagnosis were collected through chart review of the electronically medical records of the patients. After exclusion of patients with active cancer, circulating levels of each biomarker in diabetic PE patient plasma (n:90) were compared to healthy controls (n:30) and according to HbA1c levels (n:45).
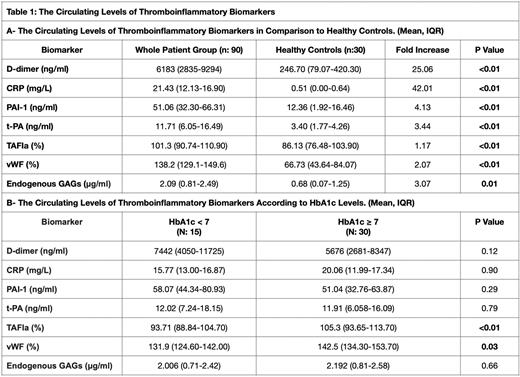
Results: The levels of all the tested biomarkers were elevated in diabetic PE patients in comparison to healthy controls (P< 0.05). D-dimer (25.06-fold) and CRP (42.01-fold) have shown the most prominent increases in comparison to healthy controls (Table 1). We did not observe any significant difference in the levels of D-dimer, CRP, PAI-1, t-PA and endogenous GAGs according to HbA1c levels (p< 0.05). The levels of TAFIa (p<0.01) and vWF (p: 0.03) were significantly higher in diabetic patients that had a HbA1c ≥ 7.
Conclusion: Our findings support that the increased levels of thromboinflammatory biomarkers and dysregulation of hemostatic pathways are important pathophysiological mechanisms in diabetic PE patients. Increased levels of TAFI and vWF may be the potential contributors of impaired fibrinolysis and endothelial dysregulation in diabetic PE patients who have poor glycemic control. These results underscore the importance of glycemic regulation in diabetic PE patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal